A little worried about your heart? You’re not alone.
Here are a four tests that you (and your doctor) ought to be looking at during your next physical.
- Omega-3 Index
- CRP (C-Reactive Protein)
- Insulin
- Triglyceride/HDL ratio
1. Omega-3 Index
I’ll have more to say to about this in a future blog, but whether you’re taking fish oil or not, you still need to know your Omega-3 index.
Why you should care: it’s a good marker of heart health.* Several studies have linked a 70 to 90% drop in risk in people with the highest Omega-3 index
It’s new, so it’s often called an ‘emerging risk factor.’
If you eat a healthy amount of fatty fish, the cell membranes of your red blood cells become enriched with Omega-3. This changes the flexibility and function of your cells.
You can measure the percent of Omega-3 in the red blood cell membrane with a simple finger prick test. You dab the drop of blood onto the test blotter and send it off in the mail. The results will be mailed back.
Acceptable Omega-3 Levels:
- Lower risk = 8% or higher
- Medium risk = 4 to 8%
- Higher risk = under 4%
The real gems in the results may be the level of Omega-6 Arachidonic Acid (AA/EPA ratio) in your cell membranes and your Omega-6 to 3 ratio. These are factors most Americans need to lower.
It is easy to boost your Omega-3 index quickly by eating fish or taking fish oil supplements. But the equally important job of decreasing Omega-6 is a very slow process and requires eliminating vegetable seed oils and reducing nuts, seeds and poultry.
You can get your Omega-3 index measured for anywhere from $30 to $99.
2. CRP (C-Reactive Protein)
C-Reactive Protein is an indicator of inflammation. CRP is released from the liver in response to inflammation.
Why you should care: it is a good predictor of future cardiac events in people who are currently healthy.
We didn’t know the predictive ability of CRP until 1997. CRP does not point to the presence of a specific disease, but inflammation is closely tied to several diseases.
Chronic inflammation of cardiac tissues and endothelium are hallmarks of poor heart health. The scar tissue from this inflammation is one of the early drivers of plaque build up.
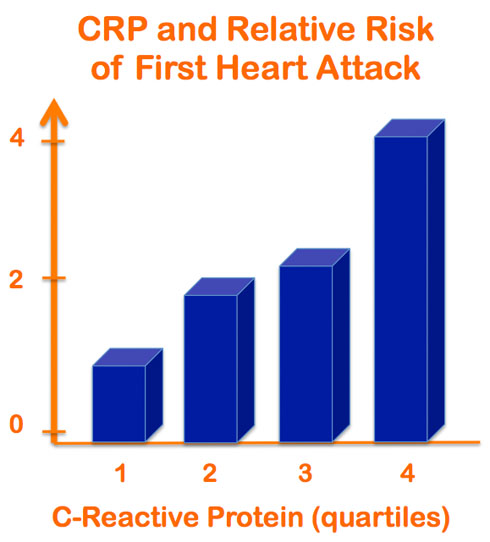
People with high CRP are up to 4 times more likely to have cardiac events and at 4 to 6 times greater risk of developing diabetes.
It’s actually a much better predictor of heart health and stroke than LDL ‘bad’ Cholesterol.
Acceptable CRP Levels:
• Lower risk: less than 1.0 mg/L
• Average risk: 1.0 to 3.0 mg/L
• Higher risk: above 3.0 mg/L
• Above 10 mg/mL usually indicates acute inflammation
It’s important to order the High-sensitivity CRP or hs-CRP test. The regular CRP test measures down to 3 mg/L whereas hs-CRP measures down to 0.3 mg/L, allowing you to detect low levels of chronic inflammation.
There are no drugs approved for lowering CRP, but some statins lower it. Several other Rx drugs lower it too, but all have significant side effects.
High CRP is a bright neon sign over your head saying ‘Time for lifestyle change.’
Diet and lifestyle factors like exercise, eating an anti-inflammatory diet (Zone, Paleo etc.), healing your gut, lowering sugar/Omega-6 can lower CRP. Using all the techniques above, I managed to get my CRP down from almost 4 to under 0.3.*
Talk to your doctor about adding this test to your panel and techniques for lowering it.
3. Insulin
Insulin is the hormone that manages your blood sugar levels and your fat metabolism.
Insulin spikes and falls based on what you eat.
Your blood has very little capacity to contain sugar. So, if you drink a glass of soda or orange juice, you’ve consumed way more sugar than what your body was built for. Excess blood sugar can give you a mild case of coma or death. To keep you from going into coma, your pancreas cranks out insulin.
Insulin then lowers your blood sugar back to safe levels. The down side? The sugar gets packed away as fat. Every time you drink a glass of orange juice, your body shifts silently to ‘Defcon 5’ and back without you knowing it.
Why you should care: 8 out of 10 people with heart attacks also have high insulin. High insulin is a hallmark of metabolic syndrome.
A diet high in sugar and refined carbohydrates will keep your insulin levels high. This leads to weight gain, high triglycerides, low HDL and small/dense variety of LDL cholesterol.
In people prone to the problem, a diet that’s consistently high in insulin-elevating sugars and carbs will lead to insulin resistance. Insulin resistance is a condition where the body ‘gives up’ and stops responding to higher and higher levels of insulin produced by the pancreas.
Like CRP, high post-prandial (after a meal) insulin levels can predict your likelihood of developing insulin resistance, pre-diabetes and diabetes. It’s easier to get your fasting insulin measured and that’s very useful too.
Measuring your fasting insulin along with your regular lipid panel is easy and your doctor ought to test it.
Acceptable Fasting Insulin Levels: Aim for 4 uIU/ml or lower. The average American is above 8.
Reducing sugar, juice, soda, grains and refined carb consumption is the best way to prevent high insulin levels. The diabetes drug metformin can reduce it. And, yes, exercise has a positive impact.
The good news: if you’re still young and/or undamaged from years of unlimited carb-feasting, going on a restricted diet like the paleo diet may drop your insulin levels quickly. In a pig study, Paleo diet dropped insulin in as little as 10 days. A few people I know fit the description, so thought I’d share. Your mileage, obviously, will widely vary.
Low-carb diets have also been shown to bring high insulin under control.
I was able to drop my sky-high insulin level down to the normal range by going on a low-carb, high-veggie paleo type diet with daily exercise. If I go on vacation and eat gelato or flan every day (Pshaw – who would do such a thing?!), my insulin (and love handles) return. Quickly. And then I look like this guy.
4. Triglyceride (TG)/HDL Ratio
Ok – this is not an actual test. Your regular lipid panel already has your Triglyceride (TG) and HDL numbers.
By dividing the Triglyceride number by the HDL you get a ratio that is very informative.
Why you should care: People with the highest TG/HDL levels are 16 times more likely to suffer a heart attack.
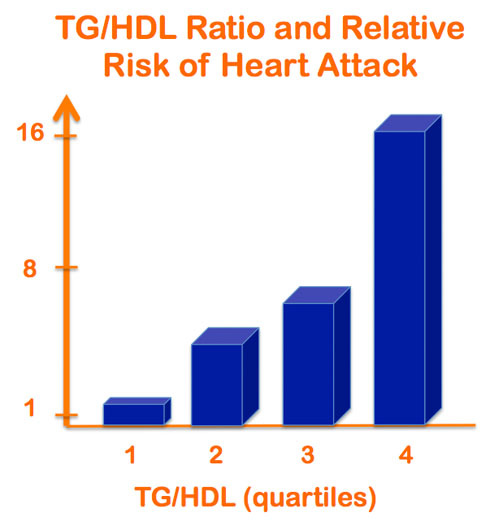
Calculating this ratio is a simple trick to measure your risk for insulin resistance, metabolic syndrome, pre-diabetes, LDL particle size and, of course, poor heart health.
High triglyceride and low HDL levels are independently good at predicting atherosclerosis. When you combine these two readily available data points, you are looking into your future with a telescope.
Small dense LDL particles are more dangerous than large ones. Measuring LDL particle density is somewhat expensive, but your TG/HDL ratio is also a poor man’s LDL density predictor. If your ratio is above 3.8, you have an 80% chance of having the more dangerous small, dense LDL. And with a ratio of less than 3.8, you have 80% likelihood of having the large, less dangerous LDL.
Acceptable TG/HDL Levels:
If your TG/HDL ratio is less than 1, you are at lower risk.
1 to 3 represents medium risk.
3 or higher may mean that you are at high risk and insulin resistant.
This ratio cuts through the confusion about ‘cholesterol numbers.’
We’ve only known about this since the turn of the century, so most doctors and lab tests don’t focus on it, even though it may be the strongest predictor of heart attack on your lipid panel.
Is it hard to get this ratio down? Yes. Mine was a sky-high 17 a few years ago. I got it down to 2.5. I’ve written about my struggles and eventual success in getting my triglyceride levels down, here and here. Simply put, it involves reducing or cutting out sugar, sodas, juices, fruits and grains.
Drugs like Lovaza can help reduce triglyceride. So can Metformin.
A low-fat, high whole-grain diet will almost certainly not work. In fact, that’s what got my ratio up to 17.
Smoking, trans fats, Omega-6 fats and fructose can all decrease HDL.
Low-carb diets are more effective than low-fat diet at getting this ratio down.
Raising HDL is harder and slower – increasing exercise, not sitting a lot, increasing healthy fats all help. Advanced HDL-boosting techniques like ketogenic diets and intermittent fasting can also help, but it will require the assistance of a professional nutritionist.
Besides these four measures, homocysteine, apoB, ferritin, coronary calcium score, and oxLDL are also good predictors of heart health. More on those another day.
*These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.



If I have low insulin producing abilities due to autoimmune disease (measured by c-peptide tests) and yet insulin is what helps drive sugar into my cells for energy and I eat a low carb diet and exercise quite a bit (often 3 mile walks in the morning and 3 mile walks in the evening), why should I have any energy at all? And if I’m insulin resistant to boot, (perhaps I’m not insulin resistant so the small amt of sugar I consume actually might get into my cells?) then you would think I would struggle immensely with energy issues. Thoughts? My endocrinologist never has given me an insulin test- for some reason he doesn’t find them helpful and prefers the c-peptide test. Any thoughts on that?
Also would pastured poultry be a source of Omega 6’s? I would think not. Industrial complex chickens – yep.
Thanks,
Mark
Hi Mark – this could easily tread into the realm of ‘practicing internet medicine,’ so I’ll keep it shallow and theoretical. I’m a bit confused with your first sentence. You don’t have to have sugar/carbs for energy. If your autoimmune condition has your insulin secretion compromised (ex T1D), you’re wise to eat a low-carb diet. Plenty of good stuff there with low-carb diet. If you were eating a Standard American Diet, I’d be worried. My guess is that if you’re consuming very small amounts of sugar and you’re walking 6 miles a day, you’re probably insulin sensitive enough for the small amount of insulin produced to push the tiny bit of glucose into your cells. If you’re having energy issues, I doubt it is from lack of sugar. It’s not unusual for endocrinologists to run c-peptide tests if a person has autoimmune-caused insulin issues – it is secondary confirmation for presence/absence of pancreatic beta cell activity.
Pastured poultry have LESS Omega-6, but poultry dark meat and eggs are still pretty high in Omega-6. With egg yolks, the benefits far outweigh the high levels of Arachidonic acid. But I try to go easy on the dark meat.
Hi Vin – My TG is at 277. I have two questions.
1. I have been reading that egg yolk contributes to TG. I eat 2 boiled eggs daily with the yolk. Please advice if I should stop eating the yolk.
2. I eat lamb (mutton) liver 4 days in a week about 100 grams per day. I recently read an article which mentioned that eating lamb liver is not good for TG.
Please advice.
Hi Ritz – sugar, starch, juices, soft drinks, grains and fruits contribute to high triglycerides. Fats and proteins have a very minor effect. Egg yolks and liver are two of the most nutrient dense foods you could eat. They wont affect your TG much. Don’t every stop eating either.
Hi Vin,
I’m a registered and licensed dietitian. Many doctors will NOT give these “FANCY” tests. My mother’s doctor got mad when I asked for a CRP.
My friend has a high cholesterol and high LDL. So her Dr recommended Statin Rx. She refused to take the Statins. But then she got a bad feeling that she should check out her heart.
She asked me what tests she should ask her Doctor to run. I said A1c, CRP, homocysteine and fasting insulin.
Her doctor refused to give all except one! He said they were all BS. But he agreed to give the A1c test. (That’s the only test that my mother’s dr also agreed was OK to give.) My friend’s A1c came back at 5.8. I recommended to cut out sugar. Then I recommended she switch doctors.
Hi Kathy – I should have added the other ‘fancy’ tests that you mentioned in the article – A1c, homocysteine and Lp(a). A1c is neither obscure nor ignored, so most doctors are happy to run that test.
There are lots of doctors who are aware of these emerging risk factors and are happy to run these tests…but most functional and integrative doctors do not accept insurance, so you may have to pay out of pocket. The doctors that do accept insurance are often too busy taking care of hundreds of patients and shoveling mountains of paperwork that they either don’t have the time or inclination to keep up with medical advances. I’d certainly expect some push back from old-school docs on tests like Lp(a), homocysteine and Omega-3 index.
I wish there was one simple, easy, cheap test to determine heart health risk with high accuracy. Such a test does not exist. Total cholesterol is a somewhat useless number, but that’s what everyone focuses on. Non-HDL cholesterol, LDL-particle number, triglyceride, LDL particle size are all far more reliable predictors of your future than Total Cholesterol. So if your doctor does not want to run the ‘fancy’ tests, at least you have non-HDL chol and TG/HDL ratio to make good decisions.
As a first line of defense, I wish doctors were more willing to push and patients more willing to accept lifestyle modifications. That’s where dietitians like you come in. Lifestyle wise, I’d like to see elimination all forms of sugar/sweets and refined grains as well as significantly increased activity, mid-day sun exposure, stress reduction and a minimum of 8 hours of sleep.
Hi Vin,
Yes, I agree with you that lifestyle is so important! My friend with the A1c of 5.8, as you know, falls into the category of prediabetes. She cut back on sugar & sweets. She just took a new A1c test & it came back as 5.5. This puts her blood sugar back into the normal range.
Sometimes it’s just that simple.
Most times, it’s much more complex.
Glad that you agree that dietitians can be helpful.
Hi Kathy – not only do I agree with you but I think most people ought to spend time with dietitians or nutritionists BEFORE the need for a cardiologist arises. But then again, most nutritionists are stuck in the 1980s, telling people to go low-fat and eat less. Oh well.
Just got some tests back today. Together with Omegavia and a Primal / Paleo eating plan (that I have been about 70% “faithful” to and started only about 3-4 months ago), my TG/HDL ratio has gone from 121/48 to 68 TG/67 HDL. So from a little over 2.5 to almost exactly 1.0. My overall cholesterol went up from 181 to 195 but since that is pretty much all because of HDL rising I am supposing that is fine. Thanks!
Wow, John, great improvements in TG and HDL. Your total cholesterol number is not different from the previous one – numbers can go up or down about 20 points on the same day if you get measured at different labs.
Hey Vin I got two more tests back (in addition to the good TG and HDL numbers above) that I just remembered the check and report … my CRP was .7 (!) and my insulin was 3.2. I have been taking your Omega 7 for 2-3 months now but I don’t have a previous CRP measurement to know if it played a part in such a good number.
Thanks!
Hi John – again, glad to hear it. Your CRP is not bad at all. Whether the Omega-7 lowered it from a higher level is a good question – very likely. A whole-food-only diet that’s friendly to your gut and your gut bacteria will likely lower your CRP a bit more. Insulin, of course, is a factor of sugar, starch, grains and fruits…and your body’s ability to process these foods.
Vin
You have correctly identified high hsCRP ( inflammation ) levels as a significant risk factor for cardiovascular events .
You might also point out that your Omegia Via product with DHA/EPA ( similar to Lovaza ) will have little effect in lowering CRP , where as your Omegia Via EPA ( similar to Vascepa ) will definitely lower CRP
Gary
Hi Gary – anything that lowers systemic inflammation will also reduce hsCRP. How EPA vs DHA affects CRP has not been adequately studied.
There are a few studies in specific populations that show Omega-3 in general reduces CRP. My approach to lowering CRP, however, would be through diet and not supplements.
A few recent references that show both EPA and DHA combined reduce CRP:
http://www.ncbi.nlm.nih.gov/pubmed/24973862
http://www.ncbi.nlm.nih.gov/pubmed/24772131
http://www.ncbi.nlm.nih.gov/pubmed/24643636
Hi Vin,
My 80 year old mother had the Omega 3 and Omega 6 fatty acid profile done. She has been taking 1 OmegaVia per day. She is trying to convince me that this is a good dose for her. I want her to take 2 OmegaVia/day. (She has pre-diabetes)
These are the results:
Omega-3 index=12.5 (optimal range >8.0%)
Total Omega-3 = 17.8 % (range .1-14 %)
Total Omega-6=24% (range 28-44%)
Omega 6 to Omega 3 ratio= 1.5:1
Arachidonic acid (AA) =12.8 % (range 10-23 %)
EPA =4.5 % (range=1%-2.5 %)
AA to EPA ratio=3:1
CRP=1.1
Fasting Insulin=6
TG=105
HDL=38
What do you think of these results? Do you have a recommendation for how much OmegaVia she should take per day?
Hi Kathy – I’d like to have these numbers when I’m 80. Kudos to your mom. May be I’d like higher HDL but that’s hard to nudge up without a lot of exercise and increasing fats in your diet. One pill seems to be doing the trick for her, which means her diet is pretty good. If she doesn’t want to take two pills, that should be OK.
My question is about my husband ,41,male(thank god 🙂 ).newly diagnosed diabetic type 2,FBS 126 mg/dl,OGTT positive with a peak at 2 hours 300,32% body fat,not very active way of life.
He is starting the zone diet to control his condition.The supplements he is taking are as follows
vit C 500
vit E 400
folic acid 500
selenium 200
chromium 200
multiminerals 1 tb
centrum 1 tb
antioxidant 8000 ORAC
aspirin 40 mg
What is the recommended starting dose for the fish oils supplement in his case?Shall we start with 3 or 5 g?
Is this OK for a diabetic and what else would you recommend?
Thanks a lot
Kate
Hi Kate – nothing is going to be better than the low-carb Zone or Paleo diet + exercise for getting his diabetes under control. I’d aim for 3 grams Omega-3 (not 3 grams fish oil), magnesium and alpha lipoic acid.
Hi Vin – I have sky high homocysteine levels along with a homozygous MTHFR gene mutation. My homocysteine has sky rocketed in the past couple years as I deal with chronic illness. I understand homocysteine is another important marker for heart disease (although you don’t discuss it much here). Most functional doctors seem to push methylated B vitamins in this case as the common protocol to reduce homocysteine. However, I seem to be very sensitive to this kind of treatment. I do tolerate your fish oil quite well. Do you know if omega 3 is indicated for reducing homocysteine? If so, what would be the correct dosage and EPA/DHA ratio? My diet is good – mostly paleo. Thanks!
Hi Joe – there is some emerging science suggesting an inverse relationship between Omega-3 and homocysteine levels, but the evidence is not conclusive. I would not depend exclusively on Omega-3 to get your homocysteine levels lower. B-vitamins are (and should remain) a better option. Perhaps you could talk to your doctor about a different source of B12, which is required to lower homocysteine levels.
Hi Vin,
I got my blood test results and below are the results that were marked as not normal. I don’t know how to interpret these results and if there any concerns. Should I change anything in my diet or take some supplements, or contacted a doctor?
Arachidonic Acid/EPA Ratio – 2.2
Omega-6/Omega-3 Ratio – 3.4
EPA – 5.2
Cholesterol, Total – 201
LDL Cholesterol Calc – 126
Thank you.
Hi Emma – I am pleased that your doctor tested your AA:EPA ratio! Very few doctors do this. The Omeag-3 numbers all look fine. Total cholesterol is not a very revealing number as that is a combination of both ‘good’ and ‘bad’ cholesterol, so 201 may be OK…you need a doctor to interpret your cholesterol numbers.
Vascepa has now been proven to lower triglycerides. Search it and the REDUCE-IT study. The FDA has now approved its use for patients with triglycerides over 150 (previously was 500). It is pure EPA (4g per day in 4 pills) highly purified, and side effects similar to placebo. The REDUCE-IT study was very robust and showed lower adverse heart events. Ask your doctor about this great anti-inflammatory natural medication.