Good news: even ultra-high doses of Omega-3 do not promote prostate cancer, says Europe’s top food safety agency.
Yet, because of a study that said fish oil could cause prostate cancer, 12 million of you stopped taking fish oil…and for no good reason.

The authors of that study have now published a new study that says ‘there was no strong evidence’ that fish oil caused prostate cancer.
‘No strong evidence’ that fish oil causes prostate cancer
The Journal of the National Cancer Institute published a study in September 2014 that, in effect, said that it was a wash. There was no cause and effect between fish oil fatty acids and prostate cancer.
Theodore Brasky and Alan Kristal, who were all over TV and radio telling us that fish oil causes cancer, are also coauthors of this new paper.
Their words, then and now:
(Keep in mind that the original study participants were not required to take or avoid fish oil supplements.)
2014: “There was no strong evidence that circulating fatty acids are important predictors of prostate cancer risk.”
This is what I had to say about it in 2013:
‘The media circus around this study plays along with this researcher’s irresponsibility and personal bias. I think the authors are aware that their data does not support these statements. It’s not ignorance. It’s just career advancement. This kind of media attention brings funding and ensures job promotions, tenureship and all-around back-slapping.
And the media? Well, fear-mongering sells. And in a facts-be-damned media circus, it’s always the supplement that gets taken out back and shot.’
The original study was not about fish oil supplements. But virtually every interview about it became about fish oil supplements.
After I published the above statement, I briefly met with Theodore Brasky, one of the authors, in February 2014. He looked uncomfortable and publicly distanced himself from co-author Alan Kristal. Yet, he continued to dig in and stand by his original unsupported statements, even though many of his more informed peers had openly criticized the study and the author’s choice of words.
This is what I have to say now:
The media should have covered this new study with as much attention as they did the sky-is-falling headline last year.
But sensationalism sells. Good news does not. (We just survived a million negative ads from the mid-term elections. I can’t remember a single positive, informative political ad. It’s what sells and it’s what gets remembered.)
So, what gives? Is the new study wrong? Or just more compatible with my preexisting bias? I don’t think the new study is wrong – it is probably a fair assessment. Science often takes a fire-aim-fire route to understanding. That was never the issue.
The issue was (and remains) the unfair coverage of health matters in the media and scientists who get caught up in the giddiness and end up making self-serving (rather than factual) statements.
12 million quitters
But what about the 12 million people who quit taking fish oil because they were afraid of prostate cancer? Most of those who quit were middle aged men and young women – two groups who critically need Omega-3 for different reasons.
Young women need large quantities of Omega-3 for pregnancy. Inadequate Omega-3 during pregnancy has serious consequences to both the mother and child.
Middle aged men are the ones most aggressively treated for heart health.
I doubt these 12 million people switched from taking fish oil supplements to eating salmon three times a week. Who is going to tell them that the media circus that made them quit fish oil is now officially inaccurate?
Do Brasky et al. owe anything to those 12 million people?
Science is a series of understandings, re-understandings and better-understandings. But that’s not what happened with Brasky et al. Their data and the author’s public interpretation of it were worlds apart.
The new paper undoes some of the scientific damage, but not the public health damage, which remains a shameful chapter in Omega-3 history. And that of Ohio State University.
Incident #2: a head-shaker and a head-slapper
Oh, the next little incident would be really funny, if it wasn’t so sad.
It involves Brian Peskin.
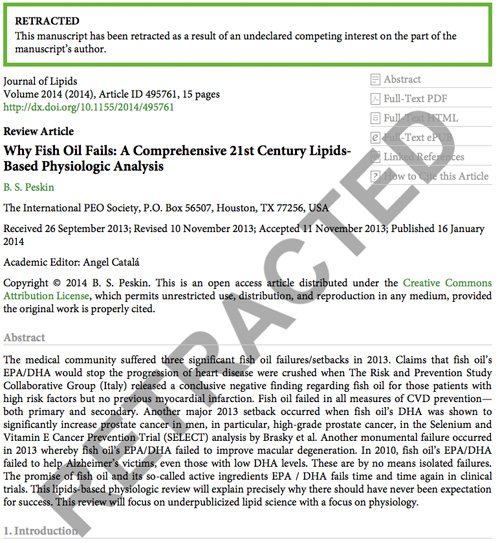
The Journal of Lipids retracted his paper titled ‘Why Fish Oil Fails: A Comprehensive 21st Century Lipids-Based Physiologic Analysis’
If you read a lot of scientific papers, that title should have made flashing red lights come on in your head.
It is rare for a journal to retract a published paper
When a retraction happens, it is usually because there was a major mistake. In this case, Peskin did not disclose a conflict of interest.
Peskin swims against the tide with his pro-Omega-6, anti-EPA/DHA stance. For reasons not fully explained in his retracted paper, he worships Omega-6 and denounces fish oil. He sells products that are rich in Omega-6 and ALA Omega-3, some of which he claims are cures for cancer.
That this business interest was not revealed by Peskin to Journal of Lipids may not be surprising, but that the editors of the journal overlooked the contents of the paper is disturbing and very puzzling.
Journal of Lipids is not exactly Annals of Internal Medicine or New England Journal of Medicine.
Journal of Lipids is a you-pay-we-publish establishment. While that alone does not nod to unethical behavior, the peer-review editors were clearly asleep at the wheel in this instance.
Here’s a list of doozies:
The unnecessary big words. The mind-numbing details about nothing that lead to nowhere. The interwoven fabric of fact and hope. Just the right amount of science to dazzle and impress average Joes all across America. (You know, kinda like this blog.) The repeated references to the now-kaput Brasky paper (see above). The out-of-place aspirational marketing language in a science journal. Citing old college text books.
The esteemed Dr. Michael Crawford sits on this journal’s editorial board. There is no chance that Dr. Crawford would have allowed the publication of this paper had he reviewed the manuscript.
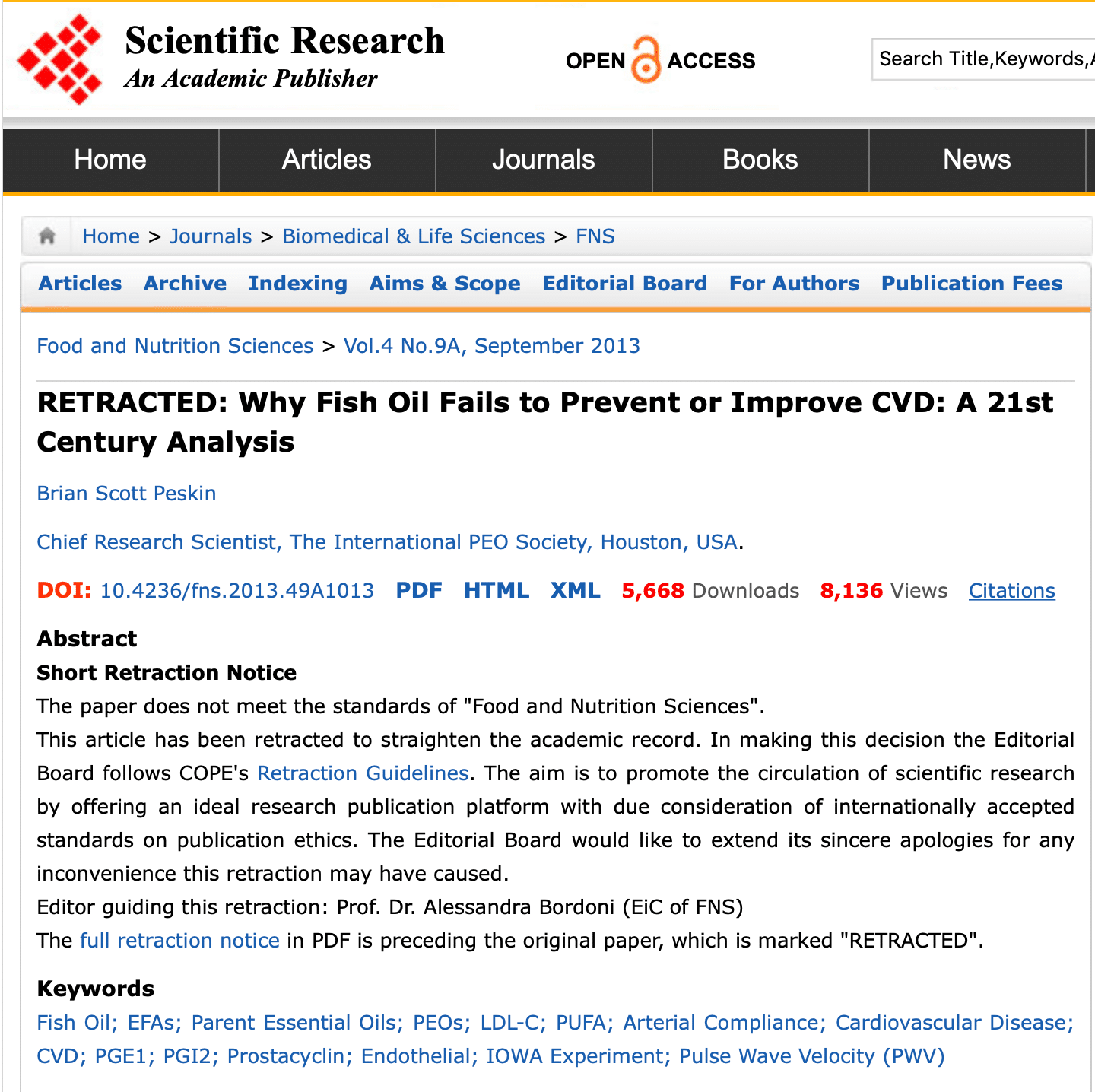
The journal’s editorial process did not vet the author’s credentials or history. A quick Google search reveals that Peskin has paid $100,000 to the state of Texas for misrepresenting his credentials and making fraudulent medical claims.
So, how did the paper get retracted?
Well, apparently several independent thinkers, including Steven Carney, contacted the publisher about the absence of real science in this paper. Canadian medical student, Ian Garber, found his ‘pseudoscience sense tingle,’ when he read the paper. So he contacted the journal about a missing conflict of interest declaration. And the editors finally (and quickly) did their jobs. Almost as if it was the first time they were reading the paper.
The missing conflict of interest statement pointed out by Garber made it very easy for the journal to retract, save face and blame-shift.
So what does all this mean to your health?
- It means that people will continue to promote their agendas, to publish papers, and to sell products, even if there is scant proof to support their positions.
- Question everything. Read a lot, not just one self-proclaimed expert. Yes, including the mindless rambling on these pages.
- Your health really is in your own hands.
And finally, know that you can never outrun disease, poor diet, and lack of exercise by taking supplements.
Addendum:
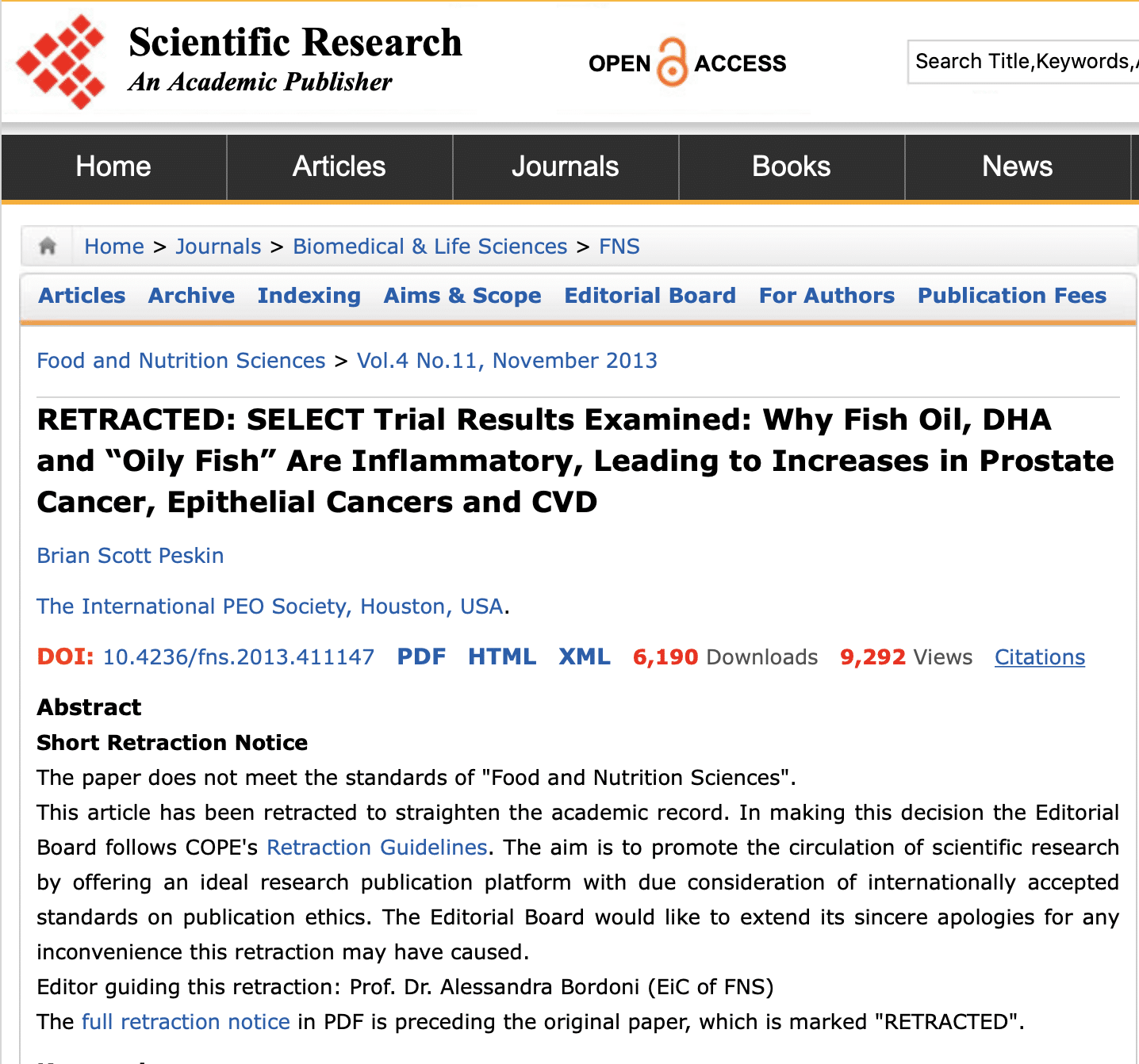
Two more papers authored by Peskin have since been retracted by Scientific Research Publishing.
*These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.



I have spoken to several people this past 18 months or so who have stopped their fish oil. Less than 1/2 of those people stopped because of the poor “studies”. Most of the people that are cutting/stopping supplements are citing the bad economy – they are struggling to keep their jobs, working several part time jobs or out of work and discouraged, with little money left for the great and healthy extras in life like supplements.
Hi Mike – of course! Those are too often the harsh (hopefully transient) realities of life. When long-time customers suddenly drop off, we sometimes reach out and we’ve found the same situation as well.
Dear Vin,
I think, a new hype was born with Krill Oil, but i didnt found extensive research material about it. Do you think is it possible the new krill oil market is taking customers from fish oil market?
Thanks to your informative blog, Im not in the group of that 12 million people.
Omega 3 is new for me, its very interesting. Your shared knowledge in these pages is the only reason, why i thought i will give a try with Omega 3. I tried so many things, nothing works very effectively so far, i was very sceptic. I am fighting joint inflammation and now taking Olimp Lab Gold Omega 3 (65% omega3/ 33%EPA, 22% DHA) The supplement box says maximum one capsule/day, but according to your site your advice is 2000mg/day (EPA+DHA) I started with one capsule, then now im taking two per day. (its 660 EPA+ 440DHA app. half of your recommended dosage)
The effect: My knee pain still here but the burning sensation disappeared. Do you think, i can increase more of this omega3 pills, lets say 3-4capsule/day and my pain can disappear? My plan is to take every 8hour one capsule, is it good? Can i use this together with diclofenac or other NSAID for a short term? In one capsule there is 12mg Vitamin E, so now im taking 24mg/day, according to a pharmacist maximum daily healthy dosage for Vitamin E is 80mg/day, so its not a problem. Do you agree with this?
Do you may have any previous posts about how EPA works against inflammation? As I understood its fighting with Arachinoid Acid.
Thanks for your help, and sorry for my english mistakes, im not a native:)
Hi Robbie – krill oil is marketed as an alternative to fish oil. As a product that has all the benefits and none of the disadvantages. So, yes, a lot of people have gone from taking 1 fish oil pill a day to 1 krill oil pill a day. This, sadly, will not give them the same benefits. Krill is a better phospholipid supplement than it is an Omega-3 supplement. So the benefits will likely be a little different.
I think you can increase your dose without issues. Take your Omega-3 with food. Every 8 hours is irrelevant. What’s relevant is that you take with food.
Each country has different threshold for Vitamin E. I can tell you that 24 mg of Vit E would not be an issue here in the US. US FDA does not consider that a high dose.
Dear Vin,
Thank you for your reply. Im fighting with this knee pain since i fell of my bike last august, visited a lot of doctors, doing physiotherapy and nobody told me i can decrease my knee pain with omega 3. Its your blog, where i found this information only, thank you!
I guess i have a joint inflammation, which effecting all my leg, im doing physiotherapy 1-2hours/day, and has ups and downs depend on the activity of the inflammation. Do you think i can combine omega 3 with kurkumin, boswellia serrata, glucosamine, hyaluron and chondroitin? Do you may have any other useful advice what can kill this inflammation?
One doctor gave me prescription Arcoxia, (its banned in the usa) but i didnt take it. Last week an orthopedist gave me diclofenac, and now from only one pill of diclofenac (no more again) I have stomach burn, i hope it can disappear, and i can start again omega3. At the moment it wouldnt be a good idea, i learned the hard way, yesterday when I took one pill of omega3 and it caused me burn in my stomach. What do you think how many days should i have to wait to start again omega3 when my stomach burn goes away? (hopefully)
Im in Poland now, and considering to buy your pharma grade omega3 to give a try. Can you ship your product to poland? Do you know is there any side effect if im taking 2g/day omega 3 for long time?
Doctors, physiotherapists, manualtherapists didn’t help me that much, then your informative blog. Thank you!
Hi Robbie – combining Omega-3 with Curcumin and Boswellia is a good idea. If your Omega-3 is causing stomach distress, stop for a few day and resume at a lower dosage or different brand. Yes, we ship to Poland, but it may take a few weeks, depending on the delays at customs.
Dear Vin,
Can I ask your opinion about this infographics?
http://www.mercola.com/infographics/fish-oil-vs-krill-oil.htm
I have the impression, this comparison is not exactly true, and im curious abour your view.
Thank you
Hi Robbie – the purpose of infographics is to convince and sell using data or convenient/manipulated data.
I would like to add these comments:
1. All fish are not toxic and full of poison like this Mercola piece would have you believe. (If fish are safe, then why buy supplements, right?) But most fish are safe…here is a list of safe fish that you can eat: http://www.omegavia.com/mercury-fish/
2. I don’t know any fish oil that contains whale or seal blubber (at least in the US). I have seen some seal oils in Asia, but they are clearly marked as seal oil. (Telling people that their fish oil contains whale is a good way to increase krill oil sales)
3. Both krill and fish oil are equally prone to rancidity and oxidation. Go ahead and try it – cut open a pill of each and leave it out in the sun for a couple of days. Smell both.
4. ’48X better’ and ‘300 times more’ are all claims that have been proven false. This is hype. I explain more here: http://www.omegavia.com/is-krill-oil-48x-better-than-fish-oil/
5. Not all fishery are exploited and over-harvested. It is easy to find Marine Stewardship Council approved fish oils and Friend of the Sea approved fish oils. The government of Peru shut down all fishery last year to maintain fish populations. (Making people feel guilty about buying fish oil is good for krill oil sales)
6. Environmental contaminants – this is a bit lower in krill. But our last batch of OmegaVia has roughly the same amount of dioxin/furans and dioxin/PCBs as the most popular krill oil product in the US. This is not the emotional message that people looking at this infographic would get. Agree?
Yess, thank you for your detailed answer! Im not a professional in this field, and this infographics was somehow suspicious for me. Im going to read more about EPA+DHA at my current stage its very useful for me. Thank you for your help, R
Dear Vin,
Im still fighting with a joint inflammation, and found an interesting article by a physician chiropractor, which states this:
“too much EPA can create oxidative stress and even inhibit healthy levels of AA, neither of which is good.”
(full article: http://sock-doc.com/2012/08/first-aid-for-injuries-part4-nsaids/)
Can I ask your opinion on this?
Thank you for your help!
Robbie
Hi Robbie – theoretically, yes, if you consume a large quantity of Omega-3 or Omega-6 fats, the double bonds in these fats can oxidize. This process happens with EPA, DHA, LA, ALA and all the other Omega-3s and Omega-6s. This is why it is always better to control inflammation with diet and lifestyle fixes than to counter high inflammation levels with equally high levels of Omega-3. If you’re talking about acute inflammation, then large doses of EPA is fine, since it will be for a short duration. But the problem is that most of us are suffering from chronic, low-grade inflammation from eating and living in ways our bodies weren’t meant for. So fighting chronic inflammation with very high doses of Omega-3, while effective, is not the best idea. Get all your Omega-3 needs with about 1000 mg of Omega-3 per day. If you need higher levels of Omega-3 to curb inflammation, then tackle the root cause of the problem. As far as the article, I have no idea why the author focuses on EPA more than other the fatty acids I mentioned above.
Dear Vin,
Thank you for your answer! Can you explain to me why not the best idea to fight inflammation with high doses of omega3? Im looking for the root of my knee pain, but still didnt found it, at the moment the new diagnosis is sartorius muscle injury with inflammation. I have another question which just makes me think: do you think accupuncture in any way can modify EPA,AA,Omega6 levels? For example if i understood clearly, massage can help to decrease cortisol levels, which is a responsible factor for inflammation. The human body is so complex, and i feel too small to understand whats going on..
Thank you for your help,
Robbie
Hi Robbie – high dose Omega-3 (more than 3 or 4 grams per day) is fine if it is for a short period of time (month or two) while you’re healing from injury or acute inflammation. This seems to be your case. But for chronic inflammation from poor diet, gut issues, lack of sleep, etc., taking high levels of omega-3 is not advised because you really need to address the root cause and you don’t want or need 5 grams of Omega-3 (or whatever) every day due to oxidation stress.
Acupuncture may help ease your symptoms, but I am not aware of any studies where it changed fatty acid levels in the body.
Eat right, tend to your injury and give it time. Don’t over think this.
Hi Vin:
I got my blood profile results and my doctor wants to put me on Atorvastatin. Here are the numbers: HDL 62, triglycerides 87. LDL 193(!). My cholesterol/HDL ratio is 4.4. (I thought one’s cholesterol level was HDL and LDL combined, but apparently not.) All other numbers unrelated to lipids were normal. Vitamin D was 58. I’m 55 and never had a cardiac event (as far as I know). I exercise almost every day. I’m not overweight and I don’t smoke. I take Omegavia fish oil and usually an Omega 7 as well. I rarely eat processed foods including cold cuts. I’m sure I could eat less carbs in the form of breads. But I almost never add sugar to my foods. I’m generally against taking any prescription drugs. I know you can’t give me medical advice, but what do you think? Do you think it would be wise to actually look into “what type” of LDL I have? I am scheduled for a stress test next week. Thanks.
Hi Brian – yes, certainly look into what LDL subtypes you have. But it may not change your doctor’s plan of action. There are lots of way to measure heart health risk. Lipid profile just happens to be a very common one. It’s not a flawed approach, because statins do help some people. I suspect you’d have less hesitation about taking statins if your HDL was 20 and your TG was 300.
Sounds like your diet is somewhat dialed in, with some room for improvement. If getting stricter on diet makes you stressed, give yourself a break.
PS: if I had these numbers, my doctor would high-five me.
Hi Brian,
I was a bit rushed in my prior post (getting ready for a dinner out with a family friend) and relied on my memory too much, so here is my corrected post. I hope I caught all the errors. My apologies.
The following might help explain your doctor’s logic. The current guidelines are heavily influenced by the Framingham risk calculators for CVD and CHD. Your numbers for CVD are as follows:
Male, non diabetic (yes?)
Age 55: 8 points (when you turned 55 you jumped from six to eight points). At age 45 you jumped from zero points to three.
Cholesterol: 4 points, the next jump is at 280 for five points, the next jump down is at 239
Non smoker: 0 points
HDL-C: 60 or higher is protective so you get:-1 points
BP: You did not give this, but as long as your systolic is < 130 you get: 0 points
Total: 11 points, or eight percent risk over the next ten years for CVD. As a male, you automatically got elevated into a higher risk category when you turned 45. However, this appears to be your only risk factor (not including LDL-C), you need two non LDL-C major risk factors to get into the more aggressive treatment category. In practical terms this means a ten percent or greater risk of CHD over the next ten years.
However, since your LDL-C was over 190, the guidelines state you should be treated with cholesterol lowering drug(s). If your LDL-C was between 160-189 mg/dL the drug(s) would be optional, but therapeutic lifestyle changes (TLC) would be initiated. If you had two major risk factors, then cholesterol lowering drugs would be started at an even lower LDL-C level. (I am assuming no family history of premature CHD.)
The TLC recommended are:
TLC Diet:
Saturated fat <7% of calories, cholesterol <200 mg/day
Consider increased viscous (soluble) fiber (10-25 g/day) and plant stanols/sterols (2g/day) as therapeutic options to enhance LDL lowering
Weight management
Increased physical activity.
(See, http://www.nhlbi.nih.gov/health-pro/guidelines/current/cholesterol-guidelines/quick-desk-reference-html)
Keep in mind this a population risk estimate, your individual risk is likely not the same. Chances are your C-reactive protein (CRP), a marker of inflammation, is low as you take omega-7 (palmitoleic acid) and CRP is believed by many, but not all experts, to be an independent risk factor. The hs-CRP should be 1.0 mg/L or lower. CRP may be more than a marker and elevated levels may be damaging.
While the Framingham data and corresponding risk calculators are widely used, it is not the only view. There was a very informative study published in 2004 in the Lancet that looked at 15152 cases and 14820 controls in 52 countries ("Effect of potentially modifiable risk-factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study"). The key lipid related factor was the ApoB / ApoA1 ratio. This ratio is more and more believed to be more accurate than HDL-C, (Tot-Chol)/HDL-C or LDL-C. It is not an expensive test and no fasting is required. (The formula used to calculate LDL-C is: LDL:C = Tot Chol – HDL-C – TG/5. Where triglycerides / 5 is used to estimate the very-low-density lipoprotein cholesterol fraction (VLDL-C). Hence fasting is required to estimate LDL-C. Note, the structural interpretation problem that arises with the above formula and the use of any risk factor that uses LDL-C, if your triglycerol levels were higher your estimated LDL-C would go down.) Preversely, if your TG had been a bit higher your estimated LDL-C would have been lower and below the 190 drug treatment threshold.
Total Cholesterol = 4.4 times HDL = 272.8,
LDL-C = 272.8-62-87/5 = 210.8 – 17.4 = 193.4 = 193, which is what you reported.
I encourage you to read the above study and discuss it with your doctor as the risk factors used in this study suggest the only risk factor you might have is a somewhat elevated ApoB/ApoA1 ratio (it correlates with LDL-C/ HDL-C). The other risk factors from the way you describe your life may be minimal. They negative risk factors are: smoking, diabetes, hypertension, abdominal obesity (not the same as high BMI, it means a a large waist), stress and high ApoB/ApoA1 ratio. The protective factors are: exercise, very moderate alcohol intake and vegetables and fruit daily. So if you have minimal stress, eat right and exercise the estimated risk will be low even if the ApoB/ApoA1 ratio is unfavorable. I think only about twenty people or so in the above study had no risk factors. Keep in mind the above study was for myocardial infarction and not specifically for the more general CVD. The above factors predicted 90 percent of the population attributable risks. This suggests that 90 percent of myocardial infarctions could be prevented.
Also, you can discuss high dose niacin instead of statins with your doctor. High dose niacin requires medical supervision. Also keep in mind that while high cholesterol is linked with CVD it is associated with longevity later in life meaning that if you don't die of CVD then sometime in your 70s or 80s it may be protective. I do not know what values are optimal for all cause mortality for various ages so the above is only conceptual and your cholesterol may still be too high.
William Lands, Ph.D. believes that if one's omega-6 levels are low (specifically HUFA omega-6 phospholipid percentage <50), then cholesterol levels are not predictive for CHD as there is so little systemic inflammation present in general. Take France and Japan, for example. The French ("The French Paradox") have low rates of CHD, but high cholesterol levels. It may be the higher and consistent intake of wine (with meals and little weekend bing drinking), daily fresh fruits and vegetables that are protective. Japanese are likely protected by their high fish oil intake—at least for those following a more traditional diet. Japanese living in Hilo, Hawaii, for example, do not have low rates of CHD.
There is some debate by some scientists whether statins are effective only because they lower cholesterol or because they are also anti-inflammatory. I read somewhere, and I may be remembering wrong, that other non-statin drugs used to lower cholesterol have not decreased mortality due to CHD; I would add that high dose niacin may be an exception to what I just wrote.
Lastly, if you decide statins are right for you consider taking CoQ10. Statins may deplete CoQ10 serum and muscle tissue levels. As we age our ability to make CoQ10 decreases.
Mea culpa, the 11 point / 8 percent calculation is for estimated risk to: “develop a heart attack or die from coronary disease in the next 10 years,” not CVD.
Robert: Thanks for all the good info! Yes, I am non-diabetic, and my sistolic ranges from 117-120, I have very little belly fat… my resting heartrate is 58-60 bpm… I’ve never heard about this correlating with CVD, but to the ignorant layperson (such as me) it seems that efficient blood pumping should indicate something about heart function. I’ve asked Kaiser if they would do an ApoB / ApoA1 ratio test. Kaiser apparently does not believe in CRP tests because every time I ask they say it is not helpful. In any case, since I appear to be just a few points above the “mandatory” threshold for drug intervention, my inclination is to see if I can get this other test done, exercise more, and eat more veggies and take the cholesterol test again… thanks, again. Brian
Hi Brian,
Aetna has a very informative web page listing all the CVD risk tests, and further it contains summaries of the various studies showing the benefit, or lack thereof, for each test.
http://www.aetna.com/cpb/medical/data/300_399/0381.html
There are many formulas using total cholesterol, HDL-C, LDL-C and TG to estimate CHD / CVD risk. Some have more evidence and studies than others.
Dr. Barry Sears (a biochemist), Dr. Sinatra (a cardiologist) and resident expert Vin (a biochemist and omega-3 expert) like TG/ HDL-C (a proxy for VLDL-C / HDL-C). Your ratio is 87/62 = 1.4, which is outstanding. A value of 2.0 (using mg/dL units) or under is optimal. Some studies (not a lot mind you, but some) show that a low TG/HDL ratio is associated (perhaps a stronger word than associated would be more apt) with larger, less dense and less harmful LDL particles.
http://www.ncbi.nlm.nih.gov/pubmed/14564088
By the study above, the odds are that you do not have the harmful LDL subclass pattern B (lots of small, dense particles). However, without directly measuring the LDL particle size you can not know for sure.
Best
Hi Robert and Brian – if I may…taking my own advice, I used strict dietary control to get my otherwise lofty TG/HDL ratio under 3. The only way I could do it was with a very low carb diet. This also made my LDL particles big and fluffy. All was good. Or so I thought. Very low carb diets have a dark side – I screwed up my thyroid hormones. It took several months to get it back to normal. Low carb diets also starve your microbiome. A very bad idea. My point: just because we know how to shift TG/HDL ratio by aggressively controlling macro-nutrient ratios, doesn’t mean it’s the right way to do it. So I’m now back to borderline TG/HDL ratios but much happier.
Hi Vin,
Sorry that I inadvertantly misstated or overly simplified your view on the TG/HDL-C ratio. That was not my intent. [Cross reference: your May 30, 2014 post: “The 4 Most Important (but Ignored) Blood Tests for Your Heart”]. It seems that choosing an ideal personal diet is a balancing act. It likely is the case for many or most people (myself included) that a diet that (forcefully) corrects one problem will likely introduce another problem.
I think the best strategy may be to choose a diet that minimizes the diseases that one is at most risk for based on genetics and family history and accept that this diet may be less optimal for preventing the other diseases that one (hopefully) is already at a low risk for. I have yet to figure out a diet that is practical and minimizes disease risk across the board. The closest may be calorie restriction, but I am even not sure about that and it is not very practical for most people.
Thank you for so generously sharing your personal dietary and medical history and your deep knowledge for the benefit of your readers. I always learn something new. It is much appreciated.
Robert
Hi Robert – I don’t think you oversimplified the TG/HDL ratio. It is simple, powerful and sadly ignored by most physicians given its predictive power. People with four-digit TG levels or diabetes still ought to go low-carb. But as you said, forceful dietary corrections become a whack-a-mole situation. It wasn’t until a couple of years after my very low carb/ketogenic diet experiment that I realized what had happened. I did not go back to a moderate carb diet because I realized that low carb was causing thyroid/adrenal issues. I simply reverted to my natural diet after a few months of experimentation and the thyroid/microbiome issues just went away. The light bulb didn’t go off until a year or two later when I was going thru some notes/medical records. This is part of the rationale in my multi-part paleo diet blog that urged paleo folks to embrace tubers and fiber. I think a TRUE ancestral diet + ancestral lifestyle probably reduces risk across the board for chronic modern diseases while increasing some infection risk. But nobody I know comes close to either of those ideals. We can’t because our environment has changed so much beyond our immediate control.
Where, and how much intensity, does an exercise program fit into your total heart and lipid health?
Regards,
Mike
Hi Mike – this is a big question, but i’ll try to keep it short. It is important to not sit. Sitting all day is not good even if you run a 5K at the end of the day. Walk a LOT. Ideally, 5 miles a day. Lift heavy things once or twice a week. Sprint occasionally. Pass on aerobic or cardio exercises. Hike up and down hills if you want to build endurance. Swim. Yoga. Definitely yoga. CrossFit ‘Lite’ one or twice a week. Ideally do all this in the mid day sun without a shirt on (kinda hard in the winter, but you get my drift.) Laugh. Hug. Have sex…may be not so much in the mid day sun.
One of my friends who is big into bodybuilding and nutrition said a doctor told him that if men lived long enough 100% would eventually develop prostate cancer. A lot simply do not live long enough to develop it.